“Sleeper” bacteria spores are like mold spores
“Sleeper” bacteria spores are like mold spores
One of the unsavory facts about mold is its ability to lie dormant when food and moisture sources dry up, until conditions allow it to “bloom” again. Scientists are finding out that there are other microbes that exhibit this same behavior, necessitating finding new ways to detect their presence.
One of these is Acinetobacter Baumannii. This superbug is usually present in wet environments, such as soil and mud, ponds, wetlands, wastewater, fish farms and seawater. Healthy people can also carry the Acinetobacter bacteria on their skin, particularly if they work in a healthcare setting. It can survive for a long time on dry surfaces, making it difficult to eliminate. (Acinetobacter: What to know)
Scientists have recently discovered a new state of “life” of this bacteria. When living conditions become too stressful, many bacteria enter a dormant state that is almost death-like, showing no metabolic activity. These are known as spores.
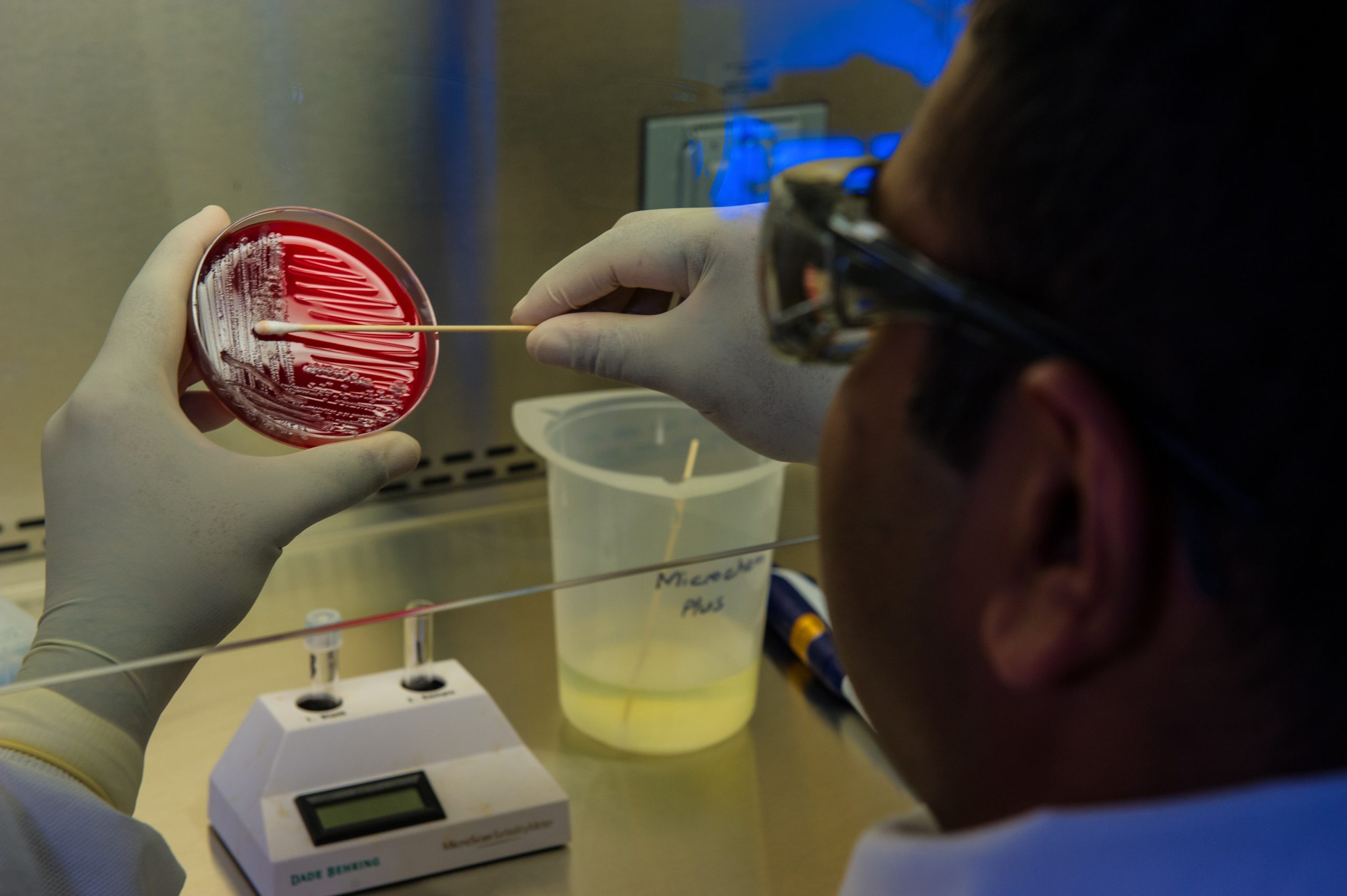
Acinetobacter baumannii can alternatively form special cells which are in a kind of deep sleep. Although these cells still show signs of life and breathe, it is no longer possible to cultivate them on culture media in Petri dishes. "We know this state from cholera bacteria, for example; it is referred to as the viable but non-culturable (VBNC) state," explains Professor Volker Müller of Goethe University Frankfurt. (The deep slumber of a hospital pathogen: Why infections with Acinetobacter baumannii can flare up again and again)
As of the study date (September 2023), scientists have kept the acinetobacter in VBNC state for 11 months, and are still able to “wake them up” after 2 days of “rehab” with special nutrients and oxygen. No end is in sight for the length of time these bacteria can hibernate.
The danger is that courses of normal antibiotics and culture procedures (on a plate) can yield negative culture results, which would indicate that a patient is clear of such dangerous microbes. However, VBNC cells can be hiding in nooks and crannies of the body, waiting to resurge when stress or antibiotics are removed Tests like PCR (Polymerase Chain Reaction) can be used to detect VBNC cells because they identify specific genes that cause virulence and predict antibiotic resistance, but it’s probable that these are not used in smaller hospitals currently.
Acinetobacter Baumannii is not the only bacteria with “sleeper” capabilities; dormancy or persistence is just a “state” that many bacteria can occupy. Mycobacterium smegmatis, which is related to the bacteria that causes pneumonia, was studied in 2013 and discovered that “persister” bacteria continued to divide and die even during antibiotic treatment so that the total number of bacteria stayed approximately the same. The fact that the cells weren’t classically “dormant” but still continued to divide, makes them technically “dynamically resistant” to antibiotics, while other microbes use other techniques to evade death and can be labeled “tolerant, latent, indifferent, dormant and non-multiplying”. (Sleeper cells – the secret lives of invincible bacteria) However, it all comes back to their ability to survive antibiotics, which is dangerous for us!
Here is some recent literature on other “sleeper cells”
Salmonella (Bacterial ‘sleeper cells’ evade antibiotics and weaken defence against infection)
Clostridioides difficile (C. diff) and weaponized anthrax (How inert, sleeping bacteria spring back to life)
E.Coli (How persister bacteria evade antibiotics, prolong infections)
Since persistent bacteria are difficult to kill with traditional antibiotics, scientists are pursuing several strategies to take them out. One is to find ways to wake all of them up, so that they are easy to kill with accessible drugs. The second is to discover what genes or proteins allow them to stay alive in sleep mode. Some of these “upregulate” cell functions (like scavenging for iron), and some of them downregulate cell functions (like digestive functions). A third tactic would be to look for drugs that kill the sleeper cells, not just active ones.
To the layman, all this sounds like poking into a hibernating bear’s den with different sticks until you find one of the right length poking in the right place, and having the best gun or trap ready for when he wakes up! The sad fact is that people regularly suffer from hosting these persistent bacteria in their bodies and we sincerely hope that scientists can find the right triggers in labs to find the combination of methods to help patients who need it.
Bacteria, mold and other microbes also populate our homes in the form of spores, persisting for years until the right moisture AND nutrients come along. Although there is no “silver bullet” like an antibiotic to remove them completely, we can use the same principles to keep the population under control so that our bodies don’t suffer!
Clean regularly with non-toxic ingredients. The less dust and dirt we allow to accumulate in our homes, the less microbe spores are lying around. Check out our article on Tackling Dust in Your Home.
The FDA states that over-the-counter antibacterial hand soaps don’t protect us from disease any better than regular soap and water. The cleansing action happens in the thorough agitation of soap and water over hands, and a good rinse with water. Many “antibacterial” soaps also contain ingredients, like triclosan, which can be harmful to us over time.
Since you can’t easily scrub and rinse items like your countertop or toilet seat with soap and water, however, different solutions need to be employed there. Sure, you can get antibacterial cleaning sprays, but the same concerns apply: are they safe long-term? Instead, opt for cleaners that are non-toxic and are less likely to create antibiotic resistance. We’ve recommended the following cleaners for these reasons:
Our all-purpose, non-toxic cleaner TotalClean combines both copper and iodine, and when they are combined, they produce peroxide! In simple terms, the peroxide acts as an “oxidizing agent”, destroying the means for bacteria to take in oxygen and suffocating them.
The Honest Company Disinfecting Spray also uses hydrogen peroxide to clean, disinfect, and deodorize while meeting EPA’s criteria for products effective against SARS-CoV-2 and a laundry list of other germs.
Because hypochlorous acid is an oxidant, it leaves nothing behind for bacteria and viruses to create resistance to and therefore does not contribute to the superbug (multidrug-resistant organisms) dilemma.(The Role of Hypochlorous Acid in Managing Wounds: Reduction in Antibiotic Usage) Hypochlorous is not bleach; in fact, it’s superior to bleach. Some hypochlorous cleaners include Force of Nature and Clean Republic’s All Purpose Cleaner.
Of course, change your HVAC filter regularly so that spores do not find their way to your air handler’s evaporator coil, where moisture can allow them to reactivate. We’ve got some great filters with activated carbon and MERV 10-14 ratings (for more on MERV, check out our article HVAC filter changes are vital to your indoor air quality.
The technology in our bipolar ionizers like our Germ Defender, Upgraded Air Angel Mobile and Whole Home Polar Ionizer has been tested against bacteria such as E. coli, MRSA and C. diff (see test results here), so why not add them to your non-toxic cleaning arsenal as a passive way to keep the spores under control?
There’s a lot about the microscopic world of bacteria and mold that we don’t know, and obsessing over it doesn’t help much! Thankfully, there are quite a few ways to keep safe using non-toxic products and methods that are tried and true.