Air quality in the Operating Room
Air quality in the Operating Room
If you are in the position to have elective surgery, you probably assume that the hospital does its best to mitigate infections by maintaining a sterile environment and using sterile procedures. The Operating Room (OR) is where patients are at their most vulnerable because hospital-acquired infections (HAIs) can easily happen when the skin barrier is broken, resulting in a Surgical Site Infection (SSI). Therefore, air quality is very important for patients’ protection, and there are a number of factors that govern the quality of the air. In the U.S., OR air quality is regulated by three organizations: the American National Standards Institute (ANSI); the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE); and the American Society for Healthcare Engineering (AHSE). Operating rooms require positive pressure, a minimum of 20 air changes per hour (ACH), with a minimum of four outdoor changes per hour. The standard specifies a minimum effective reporting value for air filter efficiency (MERV 16) but does not recommend a type of air delivery system. (Operating Room Sterilization: A Complete Guide to Air Quality) Here are some details about these requirements:
Positive or negative pressure: Traditionally, hospitals make operating rooms positive pressure in order to keep contaminants from the rest of the hospital from infecting the patient on the operating table. According to ASHRAE 170, operating rooms require positive pressurization of at least +0.01 in.w.g. However, as operations are sometimes necessary on patients who may have contagious diseases like MERS or SARS CoV-2, hospitals are beginning to rethink whether they want to put the rest of the ward at risk of spreading a microbe from a positive pressure OR room. Discussions are underway regarding alternatives such as a positively pressured OR with negatively pressured ante/setup rooms. Another possibility is to have a negatively pressured OR with positively pressured ante/setup rooms. (Rethinking air pressure in operating rooms could save lives)
The air change rate is a key factor influencing the concentration of microbe-carrying particles (MCPs). The higher exposure risks of surgical incision in the surgical microenvironment may be mitigated with increasing air changes per hour (ACH). (The impact of air change rate on the air quality of surgical microenvironment in an operating room with mixing ventilation)
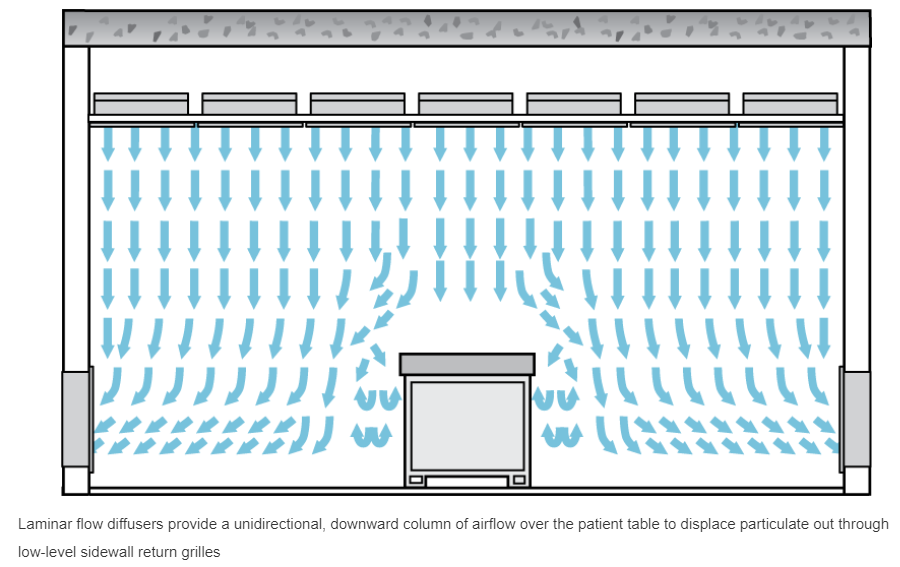
A key design requirement within ASHRAE 170 for operating rooms is the primary supply diffuser array. The airflow in the primary diffuser array should be unidirectional and downward, with an average velocity of 25 to 35 cfm per sq. ft. This is recommended with the sole intent of creating a large sterile zone around the patient and medical staff. The standard dictates that the coverage area of the primary supply diffuser array should include the surgical table and extend a minimum of 12 in. beyond the footprint of the surgical table on each side and that no more than 30% of this area may be used for nondiffuser uses (like lighting, surgical gasses, electrical outlets, televisions, etc). This recommendation ensures that enough clean, filtered air is dispensed above the patient while accommodating the complex medical equipment present in today’s modern operating rooms. (How is ASHRAE Standard 170 Applied to Hospital Operating Rooms?)
Although not it’s not mandated, it’s also a good idea to have restricted access to the OR during surgical procedures. The number of door openings are related to the number of colony-forming units (CFU) in the OR. According to this study, increased number of door openings and surgery duration increased CFU counts in the OR, but the relationship between these variables was only observed outside the Laminar Air Flow.(LAF). Within LAF conditions, only the number of staff was associated with higher CFU.
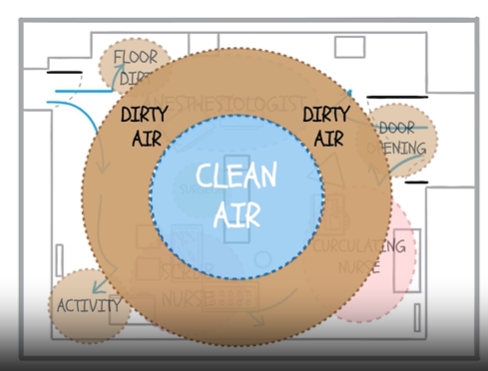
There have been several key developments in systems that promote ultra-clean operating rooms. Laminar Air Flow (LAF) systems were developed by Sir John Charnley in the 1960s for use during joint replacement implantations. They are useful for maintaining sterile conditions in the center of the operating room (under the diffusers) because they produce a continuous flow of microorganism-free air, which improves air quality by reducing infectious microbes. However, a 2023 meta-analysis agreed with multiple studies that have found it ineffective for reducing SSIs, and even possibly increasing the likelihood of SSIs, during orthopedic procedures. (Laminar airflow ventilation systems in orthopaedic operating room do not prevent surgical site infections: a systematic review and meta-analysis) In addition, air outside of the sterile field (that which is supplied by the LAF system) is often called the “dirty donut” because it is not effectively sterilized by the LAF; air in the dirty donut can be up to 100 times more contaminated than the center. There are several solutions to improving the air in the dirty donut; Aerobiotix has developed a mobile unit called Illuvia that can reduce the contaminants.
Source: Cleaning up the Dirty Donut
There is no standard for LAF design in the US. In addition to the filters employed, different sterilization devices can be employed within or outside the LAF cabinet to increase deactivation of pathogens. According to Steris, a major design/manufacture/installation firm for OR suites, the following technologies are improving LAF cabinets:
UV light: Use of mobile and ceiling mounted UV light systems is restricted to when patients and staff use full personal protective equipment. This type of light is also limited to line-of-sight, meaning that disinfection is obstructed by ceiling mounted fixtures and other equipment. UV light may also embrittle certain materials and fixtures. Therefore, in-duct UV sterilizers are preferred.
In-duct hydroxyl generator systems ultraviolet energy to produce reactive oxygen species known as hydroxyls. Airborne hydroxyls are ideal sanitizing agents which reduce pathogens and neutralize volatile organic compounds (VOC) and a broad range of chemicals. Atmospheric hydroxyls are natural-occurring molecules produced by the action of the sun’s ultraviolet energy on oxygen and water in our atmosphere. The hydroxyls are a natural oxidant and safe for patients and staff to be present during treatment without additional PPE. The system can run continuously and year-round, providing the potential for maximum surgical uptime. An added benefit is that hydroxyls help mitigate odors caused by surgical smoke and cauterized tissues.
According to this 2018 paper, it may be wise to adopt some standards of cleanrooms in ORs. One such principle is maximizing the use of ceiling space to make the ceiling one large diffuser. The reason for this is that every gap in airflow delivery (for instance, around a light connection) causes a low pressure area into which airflow is directed, producing turbulence. Therefore, the operating room would look more like this:
Source: How is ASHRAE Standard 170 Applied to Hospital Operating Rooms?
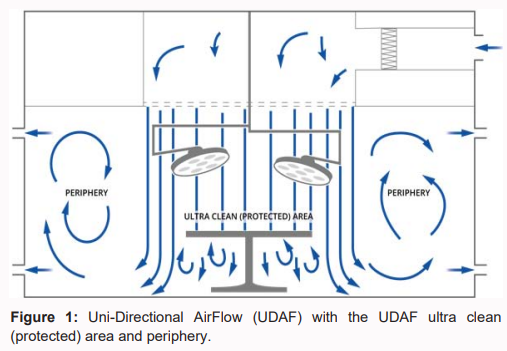
LAF is also described as Uni-Directional Air Flow (UDAF), but UDAF may not always be laminar. Here’s the difference: UDAF describes the direction of flow, however the velocity must be below 90 feet per minute in order to be described as laminar (non-turbulent). It’s easy to see that the periphery (outside the Ultra Clean Ventilation area in the center) has a lot of turbulent air flow. Although the large lights over the operating table do produce some turbulence, it is not visualized here.
Source: Air Quality in the Periphery of Operating Rooms during Surgery
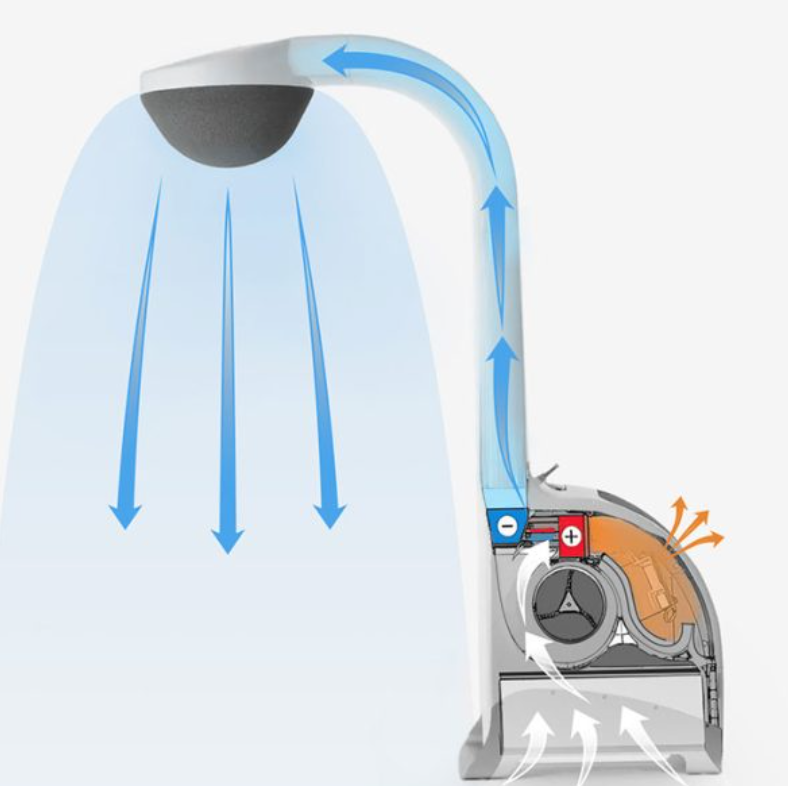
Previous LAF systems utilized fans to force air down. A new type of LAF system called Opragon was developed by the Swedish firm AvidCare, and the system uses Temperature-controlled AirFlow (TcAF). The technology behind TcAF is based on the ventilation system pumping out slightly cooled air into a zone around the operating table. By taking advantage of the fundamental laws of nature, TcAF breaks the convection currents in an effective and energy-efficient manner. Since cool air is denser than the surrounding warmer air, it drops towards the floor. The air speed is dictated by the temperature difference in the room. a temperature difference (ΔT value) of -1.5 to -3°C is required between the ultra-clean air and the ambient room air at the operating table to guarantee a fall speed of about 0.25 m/s at the level of the operating table. The technology continually checks to ensure that the ultra-clean air maintains a constant under-temperature of 1.5–3°C regardless of the temperature of the ambient room air. (Temperature-controlled AirFlow)
Air curtain systems like Mediclean emit an air curtain around the perimeter of the sterile area. The Mediclean system uses Continuous Particle Monitoring (CPM) to measure airborne particles in real-time and uses simple visual alarms. When particles are detected, Mediclean® CPM systems automatically increase the airflow from the UCV to quickly flush the contamination away from the safety-critical area, protecting both patients and surgical staff.
Other innovations include:
Surgicube, which is positioned just above the operating table, emits sterile air for minor surgeries.
Surgibox, a portable sterile surgical field with self-supporting battery and filter system
Air Barrier System, which is a portable diffuser to bathe the surgical site in ultra-clean air
A novel upward-flow design to ventilate using natural stack effect, which is less complex requiring fewer scarce components, lower maintenance commitments, lower energy requirements and operating costs.
And, it’s likely that even more innovations are in the pipeline. We thought it would be helpful to let you know that even the air in operating rooms is important for the operation’s success and your healing, so you might want to check into it if you need to have surgery!
Photo by Arseny Togulev on Unsplash