Are there any virus-detecting air sensors-out-there?
Are there any virus-detecting air sensors out there?
This is the stuff of movies: virulent strain of pandemic arrives and infiltrates everywhere except the safehouse, where a super-sophisticated detection system alerts the ventilation to shut down with sealed doors and pinpoints the germ(s), trapping them in a sticky filter and eradicating them with a non-toxic (to humans) bioweapon.
Is there such a detection system?
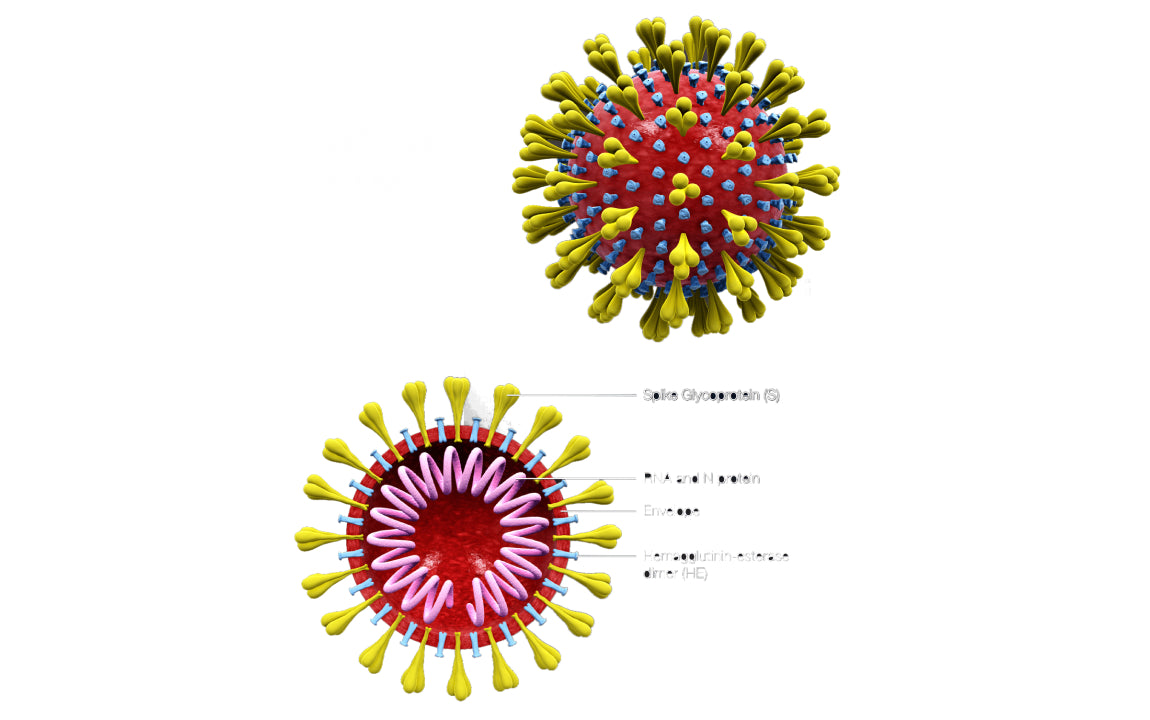
Surprisingly, there are promising sensors, one developed by Smiths Detection of the UK, which had already developed sensors for ricin and anthrax bacterium for government and courier use. Building on a technology developed by Massachusetts Institute of Technology (MIT), Smiths Detection made a BioFlash Biological Identifier that uses genetically engineered cells to bind to a toxin or antigen (like anthrax or the virus that causes COVID-19). When the cells bind to the toxin, they glow with bioluminescence, mimicking a jellyfish. Cloned jellyfish cells were the original indicators used in MIT’s CANARY technology. Smiths Detection has reported two real-world tests, in a locker room and a research facility, that showed their BioFlash SARS-CoV-2 detector is able to detect the virus that causes COVID-19 within 2-3 minutes of sampling the ambient air.
In addition,
- Baltimore company Opteev offers ViraWarn, which can be placed in offices and homes and detects dangerous spike protein viruses like SARS-CoV-2 and influenza (it cannot distinguish between the two).
- ThermoFisher Scientific has released its AerosolSense Sampler and pairs it with PCR testing (the current gold standard for identifying SARS-CoV-2 in individuals) to verify containment of the virus and support facility reopenings.
The principle of using specific agents to bind with the SARS-CoV-2 virus and causing a change in their electrical property to signal the presence of the virus, is also used in other sensors.
- One is the MedTech Actuator, in development at Royal Melbourne Institute of Technology and a biomedical startup Soterius since 2018, can detect up to eight pathogens in one sensor. This sensor, known as “The Scout”, could be worn or placed on a wall in a reception area, for example.
- Recently researchers at the Yale School of Public Health released a wearable clip that can detect low levels of SARS-CoV-2, to alert the wearer if they’ve been exposed. It’s called the “Fresh Air Clip” and it’s not available publicly yet.
- Researchers at the Swiss Federal Laboratory have developed a thermal and optical-based sensor that uses gold nanostructures on a glass substrate, to mimic DNA receptors to identify the virus in the air. (medicaldesignandoutsourcing.com)
While virus-detecting-air-sampling equipment is not widely accessible yet, leading air sensor companies like AirThings are taking steps to determine the next best thing: the risk of virus transmission in buildings. If the presence of a virus is unknown, the risk of transmission is something that can be managed. It is known that virus particles are transmitted by direct contact, but also through microdroplets, or aerosols. Microdroplets are expelled with every breath of a person and can float in the air for extended periods of time. These droplets are so small–on the order of a hundred millionths of a meter–that they are too small to be seen by the naked eye, and much smaller than the “spray” that is seen when someone coughs or sneezes. Microdroplets are able to float on currents of air in our space, in the right conditions, for hours. The longer the microdroplets persist, the more concentrated they can become in a space, and the more people they would have the opportunity to infect. Airthings’ sensors are therefore arranged to measure the supporting conditions allowing the microdroplets to persist: carbon dioxide (CO2), temperature, and humidity.
CO2 levels are a direct measurement of the number of people in the space and its ventilation. If CO2 rises with constant ventilation, then the sensors would know that more people have entered the space. According to ohsonline.com, the normal level of CO2 outside is 250-300 parts per million (ppm), and up to 1,000 ppm CO2 can be considered a good air exchange for buildings. When the level rises above 1,000 ppm, people start to sense that the air seems stale and/or they become drowsy. This is when there are simply too many people, or too little ventilation, or both. If an infected person is in this poorly ventilated space, this type of condition will allow microdroplets of virus to build up, increasing risk of infection.
Other than CO2, two more factors are considered: temperature and humidity. The higher the temperature, the less likely viruses are to survive for longer periods. Likewise, low humidity helps microdroplets to float even longer, because it makes them lighter. Viruses need very little moisture to survive and remain encapsulated, so the less moisture in the microdroplets, the lighter they become and more easily moved by air currents. Here is where the risk doubles: cooler, dryer air also lowers our own ability to fight off infection. Cold air, dry air causes an inflammatory response in the lungs of people with COPD and asthma, even with changes as little as 2-3 degrees (like walking into a building with air conditioning in the summer). Even in people with no respiratory conditions, breathing in dry air tends to evaporate the airway surface liquid (ASL), which is an important defense against infection.
Having identified the ranges of these risk indicators, then a smart system with sensors can also be programmed to suggest ways to lower the risk. These could be to lower the number of people in the space, or increase the temperature and humidity, or a combination of all three. No matter if the risk is COVID-19, or flu, the rewards of being cautious can be precious.